Do I Have a Psychotic Disorder?
Psychotic disorders are a group of mental illnesses that share similar symptoms revolving around abnormal thinking.
They all have the shared symptom of psychosis, though not everyone with a psychotic disorder experiences psychosis, and not everyone with psychosis has a psychotic disorder.
While ordinary psychosis may be triggered by stress, illness, or substance abuse, psychosis in someone with a psychotic disorder is one of the well-known symptoms, and it may come and go without external factors influencing it i.e., it is caused by mental illness and nothing else.
The mental illnesses that come under psychotic disorders are:
- Delusional disorder
- Paraphrenia
- Schizophrenia
- Schizophreniform disorder
- Schizoaffective disorder
- Substance-induced psychotic disorder
- Brief psychotic disorder
- Psychotic disorder due to a medical condition
If you may be suffering from psychosis due to addiction issues, get help by calling our team on 0800 088 66 86
Different Types of Psychotic Disorder & Their Symptoms

Below, we discuss the different types of psychiatric disorders and their associated symptoms:
1. Delusional disorder
Delusional disorder is marked by an inability to distinguish reality from one’s imagination. Sufferers can have wildly unrealistic delusions, such as being a world leader or being taken by aliens.
These are known as ‘bizarre delusions’, as they are not a reflection of the individual’s genuine life experiences or current circumstances.
On the other hand, some delusions are more closely associated with reality. Some people with delusional disorder believe certain people are in love with them, believe everyone is conspiring against them, or they are being followed by strangers.
The reason these delusions are less bizarre is that they do happen in real life more frequently, but they are still delusions as they are not happening to the individual concerned.
There are six main types of delusion in delusional disorders, and these are:
- Grandiose: Someone with grandiose delusions tends to believe they are superior to others, in terms of education, knowledge, identity, power, and general worth.
- Jealous: Jealous delusions often revolve around being cheated on by one’s partner.
- Somatic: People with somatic delusions may sincerely believe that they are suffering from a medical problem, despite being in good health.
- Mixed: People with mixed delusions can experience two or more of the different types of delusion.
- Persecutory: Persecutory delusions centre around being harmed by someone.
- Erotomanic: This delusion is marked by the belief that someone is in love with the patient.
Delusional disorder used to be called paranoid disorder, which gives you an insight into the experience of people with this disorder – they are often paranoid about negative things happening to them.
The most common demographic for delusional disorder is women in their later life, but this condition can affect anyone.
It can be very difficult to spot delusional disorder, as many people with this illness only exhibit symptoms when they are faced with their delusion.
For example, they may become extremely paranoid and aggressive when they are at a family gathering where they believe they are being conspired against, but they could attend a social event with friends quite happily without showing any symptoms.
Psychiatrists can diagnose delusional disorder if they see symptoms in patients such as hallucinations, delusions and low mood.
2. Paraphrenia
Paraphrenia is a mental disorder characterised by paranoid delusions.
It is very similar to schizophrenia, but it affects a different group of people. While schizophrenia can affect a wide range of age groups, paraphrenia tends to affect people over the age of 60.
Furthermore, paraphrenia tends to have an obvious trigger.
The two main triggers are stressful personal situations (emotional trauma) and severe neurological illnesses (blood vessel damage, nerve damage, stroke, tumour, serious injury).
As many of the symptoms of paraphrenia overlap with schizophrenia and delusional disorder, paraphrenia is often misdiagnosed as another psychotic disorder.
However, one clear difference between paraphrenia and other psychotic disorders is that patients do not deteriorate as quickly.
Another difference is that paraphrenia does not seem to have as strong of a genetic component as schizophrenia.
The main symptoms of paraphrenia are:
- Hallucinations
- Perceiving strong smells despite there being no smell
- Perceiving noises/voices/sounds that aren’t there
- Paranoid delusions
It is important to note that not every medical professional agrees that paraphrenia is a separate illness to schizophrenia or delusional disorder, and as such this psychotic disorder does not appear in the DSM.
Talk with our team today by calling us on 0800 088 66 86
3. Schizophrenia
Schizophrenia is one of the most common psychotic disorders, and it tends to affect young people.
It is mostly diagnosed in female patients who are in their early thirties and male patients who are in their early twenties, though the illness is likely to have existed for a while before the diagnosis.
The most common symptoms of schizophrenia are:
- Disorganised thinking: Some people with schizophrenia struggle to get their thoughts in order, and this presents as disorganised speech e.g., unintelligible sentences or unrelated answers to questions. It is important to rule out other conditions before attributing schizophrenia to this symptom, as it can also be a sign of drug use, liver failure, bipolar disorder, or dementia.
- Hallucinations: Just like many other psychotic disorders, schizophrenia is likely to cause hallucinations. Patients can see things that aren’t there or hear sounds that haven’t been made. A common example you may have heard of is a schizophrenic patient hearing voices in their head.
- Unusual motor behaviours: This symptom is subjective, but if someone is suddenly exhibiting unusual motor behaviours, it may be a sign they are dealing with schizophrenia. Some examples of unusual motor behaviours are: excessive movement, unresponsiveness, spasms, and pacing back and forth.
- Delusions: The delusions experienced in schizophrenia can be the same as the ones in delusional disorder. This means they may revolve around being unsafe, being targeted, being admired, or being superior to others.
- Low mood: Low mood is sometimes a feature of schizophrenia, and it may be discovered due to a patient withdrawing from others, neglecting personal hygiene, losing interest in things they once enjoyed, or not showing emotion.
- Schizophrenia is a very dangerous mental health condition as it is linked to premature mortality. It is predicted that schizophrenic patients lose 28.5 years of their life on average due to their illness.
The usual risk factors of mental illness apply to schizophrenia, which include trauma, genetics, and other mental health conditions. However, schizophrenia is also closely linked to the use of mind-altering substances, particularly if they are taken at a young age.
Taking LSD, cocaine, cannabis, or amphetamines can cause some people to develop symptoms of schizophrenia, even if they have no previous history of mental illness.
Birth complications have also been linked to schizophrenia. People who did not get enough oxygen during birth, were born premature, or had a low birth weight are more likely to develop schizophrenia.

4. Schizophreniform disorder
When an individual has schizophreniform disorder, they have the same symptoms as schizophrenic patients, but the symptoms are more short-lived.
They tend to last up to six months.
Patients with schizophreniform disorder may experience:
- Hallucinations
- Disorganised thinking
- Bizarre behaviour
- Loss of interest in everyday activities
- Delusions
- Poor hygiene
- Social withdrawal
- Alack of energy
This disorder is diagnosed in men at a younger age than women, though it affects both genders equally. Men are most likely to be diagnosed between 18-24 years of age, whereas female diagnoses occur more often between 24-35 years.
Though the symptoms of schizophreniform disorder clear up within six months, the impacts of this disorder may last for a very long time.
This is because people’s lives can turn upside down when they first develop this disorder.
For example, as a result of hallucinations and delusions, patients may have to give up work, let go of relationships, and even enter a treatment centre to manage their symptoms. When their symptoms go away, they have to deal with the fact that they have lost close friends, lost their job, and spent time away from general society.
This can cause people to develop poor mental health, as they are depressed about how their life has turned out, and they are stressed about how they are going to get it back on track.
To discover how a rehab service can help you, give our team a call on 0800 088 66 86

5. Schizoaffective disorder
This psychotic disorder features symptoms of both schizophrenia, and mood disorders (e.g. depression or bipolar disorder).
There are three types of schizoaffective disorder: depressive type, bipolar type, and mixed type.
All of these types feature symptoms of schizophrenia.
Some of the symptoms that overlap with symptoms of other psychotic disorders are:
- Bizarre behaviour
- Speech problems
- Delusions
- Low mood
- Hallucinations
However, some symptoms are unique to schizoaffective disorder, including manic episodes (having a boost in energy that prevents sleep and lasts for days at a time) and depressive episodes (losing interest in everything, feeling numb and empty).
Just like schizophreniform disorder, schizoaffective disorder is just as likely to affect women as men, but men develop the disorder earlier in life. This disorder is very rare, with only 0.3% of people suffering from it.
A diagnosis of schizoaffective disorder requires the patient to show symptoms of both a mood disorder and schizophrenia. What’s more, there must be evidence of two or more psychotic episodes lasting at least two weeks.
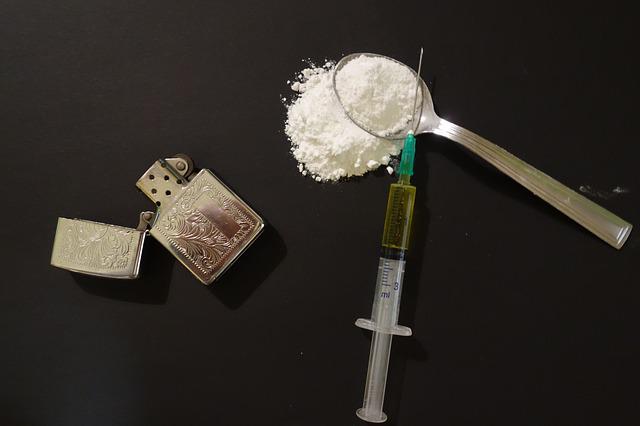
6. Substance-induced psychotic disorder
As we have discussed, psychotic disorders can be linked to environment and genetics. However, they can also be caused by substance use.
When an individual mixes substances, withdraws from a substance, uses drugs while having mental health issues, or takes a very high dose of a particular susbstance, they may experience substance-induced psychotic disorder.
There are many reported cases of people with substance-induced psychotic disorder being later diagnosed with schizophrenia.
The most common substance that leads to a diagnosis of schizophrenia is cannabis.
However, there are many other substances that have been linked to substance-induced psychotic disorder, including:
Medication can also be linked to this disorder, with particularly problematic medications including:
- Antipsychotics
- High-dose antihistamines
- Antidepressants
- Antiepileptics
- Antimalarials
- Cold medications
As you can see, over-the-counter and prescription drugs alike can cause substance-induced psychotic disorder.
Perhaps surprisingly, even nonmedicinal substances can be a cause. This includes:
- Antifreeze
- Heavy metals
- Arsenic
- Sarin
- Carbon monoxide
- Carbon dioxide
- Carbon disulfide
- Organophosphate insecticides
- Aniline
- Acetone
Most cases of substance-induced psychosis are resolved within a few hours, as the symptoms go away when the individual is no longer under the influence.
However, in some instances, this disorder can last for weeks or even longer.
Given that many substances can cause symptoms of hallucinations, it may be hard to distinguish between an ordinary reaction to drugs and substance-induced psychotic disorder – particularly if someone is taking a new drug for the first time.
However, the symptoms should be compared against the patient’s usual reaction to drugs.
If someone usually only experiences dizziness and headaches, and they are suddenly experiencing delusions, substance-induced psychotic disorder should be considered as a potential cause.
Learn more about how addiction can induce psychotic disorders by calling us on 0800 088 66 86

7. Brief psychotic disorder
Brief psychotic disorder is the presence of psychotic symptoms that occur after a stressful event and goes away after a short period of time.
Some people are not even aware that they have had an episode of psychosis when they suffer from brief psychotic disorder.
Some life events that can cause brief psychotic disorder are:
- The loss of a loved one
- Divorce
- Job loss
- Poverty
- Chronic illness
- Financial troubles
- Mental health struggles
This type of psychotic disorder is much briefer than the others, as it only lasts from one day to one month.
If symptoms persist, other psychotic disorders must be investigated e.g., schizophreniform disorder or schizophrenia.
One example of brief psychotic disorder is when women experience a psychotic episode after giving birth, which can last up to one month.

8. Psychotic disorder due to a medical condition
As the name would suggest, psychotic disorder due to a medical condition is a type of psychotic disorder that only occurs when someone is suffering from a medical condition. This can be a temporary experience, such as a migraine, or a long-term chronic illness.
Sometimes, this type of psychotic disorder is misdiagnosed as schizophrenia, as the symptoms overlap.
The main symptoms include disorganised thoughts, delusions and hallucinations.
However, it is important to look at the medical history of patients to determine whether their psychosis is coming from a mental condition, or if it is a symptom of a medical condition.
One medical condition that has been closely linked to psychosis is epilepsy. 4-7% of people with this condition will experience psychosis, which rises to 7-11% if they have temporal lobe epilepsy.
Some risk factors for psychosis among people with epilepsy are:
- Abnormalities in the left hippocampus
- Cognitive impairments
- A history of status epilepticus
- Hippocampal sclerosis
- Cell loss in the CA1 region
- Having epilepsy before the age of 10
Give our expert team a call today on 0800 088 66 86
What Causes Psychosis?

Long-term psychosis is likely to be associated with a psychotic disorder, such as the ones listed above.
The causes of this are not confirmed, as there are still studies into whether mental health conditions are more closely associated with nature or nurture.
Though the theories vary, some commonly accepted causes of long-term psychosis are:
- Trauma
- Genetics
- Abuse
- Grief
- Neglect
- Prolonged (or sometimes even short-term) use of recreational drugs
When people take drugs over a long period of time, if they are already vulnerable to experiencing psychosis, they may begin to deal with some of the symptoms of psychosis e.g. delusions and hallucinations.
In some cases, it has been known for one-time drug use to lead to psychosis. This is called drug-induced psychosis.
It is more likely to occur when someone mixes drugs or takes a large dose of a drug.
Physical illness is another potential cause of psychosis, as we have discussed previously. This can either be a short-term experience that does not reoccur or a long-lasting disorder that requires medication.
In some instances, prescribed drugs for certain illnesses can be a cause of psychosis.
Some drugs that have been known to cause psychosis are:
- PCP
- LSD
- Scopolamine
- Ketamine
- Isotretinoin
- Amphetamine
- Corticosteroids
- Benzodiazepines
- Antiepileptic drugs
- Opioids
- Fluoroquinolones
- Antidepressants
- Anticholinergic drugs
There are a few situational factors that can increase your likelihood of experiencing psychosis, though they are unlikely to be the sole cause.
These are not getting enough sleep and not eating enough.
If you do this over a long period of time, you could potentially have a psychotic episode.
Spiritual experiences are another possible cause of psychosis, though this is a controversial theory.
Some people claim to experience hallucinations as part of a religious experience, and they do not believe it is linked to mental illness as it is a positive experience.
When are Psychotic Disorders More Likely to Develop?

It is rare for psychotic disorders to emerge in childhood.
One study found that most people with a psychotic disorder first experienced symptoms in their late teens to early twenties. Later onset is not uncommon, but it is more likely to be linked to a secondary cause, such as a medical condition.
When we look at schizophrenia, which is one of the most common psychotic disorders, the average age of diagnosis is 24 years old.
The youngest recorded age is 3 years old, and the oldest is 63 years.
Men are more likely to be diagnosed, or to experience symptoms, in their late teens. On the other hand, women are more likely to be affected in their late twenties.
Think you might develop a psychotic disorder? Chat with an expert today on 0800 088 66 86
Who is More Likely to Develop a Psychotic Disorder?

People who are genetically prone to developing a psychotic disorder are the most at risk.
It is estimated that psychotic disorders have a heritability of 85%. In other words, 85% of the chance of developing a psychotic disorder is determined by one’s genes.
It is not always easy to know what our heritability is, but if psychotic disorders run in your family, you are much more likely to develop one.
For example, if your parent has a psychotic disorder, you are 7.5 times more likely to develop one yourself.
A 2016 Adult Psychiatric Morbidity Survey discovered that 0.7% of people living in the UK had a psychotic disorder. It occurs most in black men, with a prevalence of 3.2% .
Other people who are more prone to developing a psychotic disorder are:
- People who use drugs heavily
- People who have experienced severe trauma
People who do not sleep enough - People who take a medication that has psychosis as a side effect
What is Postpartum Psychosis?

Postpartum psychosis is a type of psychosis that affects women who have recently had a baby.
It is normal for women to experience low mood just after giving birth, and we often refer to this as the ‘baby blues’. In most cases, this will only last for several days.
However, some women go on to experience postpartum psychosis, which has much more dangerous symptoms, and can persist for a significant length of time if left untreated. It affects 1 in 500 new mothers.
Women are more likely to experience postpartum psychosis if they have dealt with psychosis in the past, they have a history of mental illness, and they have a history of postpartum psychosis with a different child.
If you treat postpartum psychosis immediately, the most severe symptoms should either disappear or reduce in severity within three months (though in some people, it can be as quick as two weeks).
However, there are cases of this disorder lasting up to 12 months. Usually, women experience a reduction in symptoms within the first few weeks or months, but a full recovery may not happen until much later on.
Find your way towards better mental health by calling our team on 0800 088 66 86
Do I Have a Psychotic Disorder?

You may have a psychotic disorder if you are experiencing delusions and hallucinations.
However, you need to speak to your GP before self-diagnosing, as the symptoms can overlap with other mental illnesses.
What’s more, if you do have a psychotic disorder, it is important to find out which one you have so that you can get the appropriate treatment.
Please remember that psychosis is not the same as psychopathy. Psychopathy is an antisocial personality disorder, with symptoms including a lack of empathy and being manipulative.
On the other hand, psychosis is not a personality disorder, so there is more treatment out there, and it is very likely that people will recover from psychosis.
Treatment For Psychotic Disorders

One treatment for psychotic disorders is therapy. Though this cannot prevent you from experiencing psychosis completely, if you are in a better mental state then you are less likely to experience severe symptoms.
Moreover, you will gain a better understanding of your disorder, which could prevent you from developing low self-esteem as a result.
Cognitive behavioural therapy is a common type of therapy associated with psychotic disorders, but holistic therapies and counselling can also produce great results.
Finally, you can take medication for psychosis, which reduces the severity of symptoms. The most common type of medication prescribed to people with a psychotic disorder is antipsychotics.
They can be prescribed by psychiatrists, specialist pharmacists, specialist nurse prescribers, and GPs.
Antipsychotics work by blocking dopamine, as one theory of psychosis is that it is caused by an overproduction of dopamine.
There are some side effects of antipsychotics, as is the case with every type of medication. However, most people do not experience dangerous side effects.
Some examples of side effects that can be caused by antipsychotics are:
- Blurred vision
- Weight gain
- Restlessness or akathisia
- Constipation
- Tardive dyskinesia
- Dry mouth
- Drowsiness
- Sexual issues
- Hyperprolactinaemia
- An increased risk of diabetes
If you would like to learn more about the various treatment methods used to address psychotic disorder, give our team a call on 0800 088 66 86
Can You Recover From a Psychotic Disorder?

Fortunately, it is very common for people to recover from psychotic disorders.
Most people will recover after their first treatment, which usually includes antipsychotics and therapy.
However, this does not happen overnight.
It tends to take several months before patients report experiencing zero symptoms of psychosis.
When left untreated, psychosis can last for many years. It is vital that you see a doctor as soon as you experience any symptoms of psychosis, as this is the best way to recover as quickly and safely as possible.
Get Help With Rehab Recovery

If you have a psychotic disorder and the initial treatment is not adequate, you could consider attending rehab. You will be able to continue to take antipsychotics and continue with therapy, but in a controlled setting that increases your chances of recovery.
Psychosis can be worsened by stressful life experiences, so if you go to private rehab, you will get a break from any big stressors in your life, and this could be just what you need to help you recover.
It is not guaranteed that completing treatment in rehab will cure you of your symptoms, as symptoms do persist in some people.
However, it is likely to reduce the severity of your symptoms and help you to function well in society despite your struggles.
To find a place at a rehab centre near you, get in touch with us on 0800 088 66 86





